Today in Morning Report, we discussed the differential diagnosis of lymphadenopathy. Broadly, one should consider the following etiologies:
- Infectious (bacterial, viral, mycobacterial, fungal, protozoal, spirochete)
- Malignancy (primary vs. metastatic; hematologic vs. solid)
- Lymphoproliferative (hemophagocytic lymphohistiosis)
- Immunologic (serum sickness, drug reactions)
- Endocrine (hypothyroid, Addison's)
- Other (sarcoidosis, SLE, rheumatoid arthritis)
When you first approach such a presentation, it is important to differentiate between localized and generalized lymphadenopathy.
Localized lymphadenopathy involves typically only one of the following lymph node regions:
Cervical: systemic infection (EBV, CMV, toxoplasmosis,TB), lymphoma, head and neck malignancy.
Supraclavicular: right-sided (associated with thoracic malignancies), left-sided/"Virchow' node" (associated with intraabdominal malignancies).
Axillary: local infection (cat scratch disease), malignancy (breast).
Epitrochlear: palpable epitrochlear lymph nodes are always pathologic, differential diagnosis includes infection, lymphoma, sarcoidosis, secondary syphillis.
Inguinal: lower extremity infection, STIs, malignancy.
Generalized lymphadenopathy is commonly a feature of a systemic disease, including:
HIV: in acute, primary infection, typically non-tender.
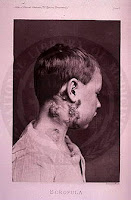
Mycobacterial infection (tuberculous and non-tuberculous): called "scrofula" when it involves lymph nodes alone, typically the neck.
Infectious mononucleosis: classic triad of fever, lymphadenopathy, and pharyngitis.
SLE: more frequently noted in acute presentation or exacerbation of disease.
Medications: often associated with "serum sickness" (fever, arthralgias, rash, generalized lymphadenopathy), e.g. allopurinol, atenolol, antiepileptics, hydralazine.
Uncommon causes include: Castleman's disease, Kikuchi's disease, Kawasaki disease, amyloidosis.
A lymph node biopsy:
- can be considered if an abnormal node has not resolved after four weeks.
- should be performed immediately in patients with other findings suggesting malignancy (fever, chills, night sweats, unintentional weight loss).
- open lymph node biopsy is preferred, if feasible.
Check out this NEJM Images in Clinical Medicine for a less than subtle presentation of axillary lymphadenopathy: http://www.nejm.org/doi/full/10.1056/NEJMicm071065.